Blood Counts
Blood Counts
Blood Counts
Your child’s neuroblastoma treatment can impact the number of cells in their blood, so it is important for the healthcare team to monitor their blood counts throughout treatment.
To do this, your child’s healthcare team uses a laboratory test called a complete blood count (or CBC) to measure the number of blood cells in your child’s body. During neuroblastoma treatment, they will focus on the following aspects of your child’s CBC:
- Absolute neutrophil count—measures how many neutrophils are present
- Hemoglobin and/or hematocrit—measures how many red blood cells are present
- Platelet count—measures how many platelets are present
Potential causes of low blood counts
Certain neuroblastoma treatments, such as chemotherapy, radiation, and antibody therapy, can affect the bone marrow’s ability to make blood cells. It is common for a child with cancer to have low blood counts after receiving treatment. With chemotherapy, neutrophil counts are usually at their lowest 7 to 14 days after the therapy is given.
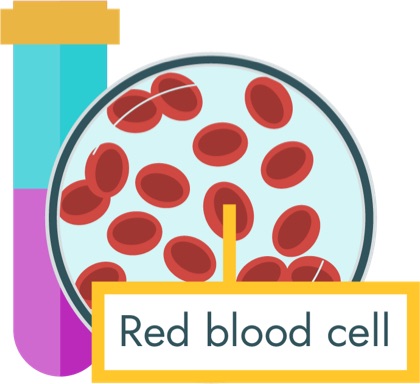
Low red blood cell count (anemia)
Red blood cells help carry oxygen in the body. Your child’s healthcare team will measure the red blood cells by checking the hemoglobin (Hgb) and/or hematocrit (Hct) as part of the CBC. When your child’s hemoglobin and hematocrit are low, it is called anemia.
Signs and symptoms of anemia
If your child is anemic, they may develop the following symptoms:
- Pale skin
- Pale gums
- Feeling tired
- Dizziness
- Sleeping more and playing less
- Headache
- Fast heart rate
Treating anemia
If your child’s red blood cell count is too low, your child’s healthcare team may order a blood transfusion. During a red blood cell transfusion (also called packed red blood cells or PRBC transfusion), red blood cells will be given through your child’s central line.
The transfusion is usually given over 2 to 4 hours. Your child will be closely monitored during the transfusion. It is very common to receive blood transfusions during cancer treatment.

Please call your child’s healthcare team if your child is dizzy or light-headed, or if you are concerned and think they may need a blood transfusion.
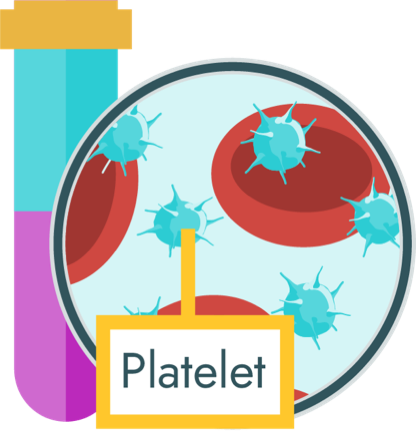
Low platelet count (thrombocytopenia)
Platelets help stop bleeding by forming clots. Your child’s healthcare team will check the platelet count as part of the CBC. When your child’s platelet count is low, it is called thrombocytopenia.
Signs and symptoms of thrombocytopenia
If your child is suffering from low platelets (thrombocytopenia), they may develop the following symptoms:
- Bruising
- Tiny red spots on the skin (also called petechiae)
- Nosebleeds
- Bleeding gums
- Bleeding from the central line
- Blood in the urine, stools, or vomit
Treating thrombocytopenia
If your child's platelet count is too low, their healthcare team may order a platelet transfusion. During a transfusion, platelets will be given through your child’s central line. The transfusion is usually given over 1 to 2 hours. Your child will be closely monitored during the transfusion. It is very common to receive platelet transfusions during cancer treatment.

Please call your child’s healthcare team if your child has unusual bruising or if their bleeding won’t stop.
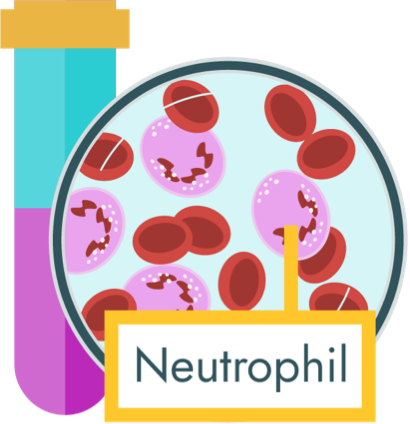
Low neutrophils (neutropenia)
Neutrophils are white blood cells that play an important role in defending your child’s body from infection. Your child’s healthcare team will check the absolute neutrophil count as part of the CBC. When the neutrophil count is low (less than 500), it is referred to as neutropenia.
Signs and symptoms of neutropenia
Often, there are no outward signs and symptoms of neutropenia. However, if your child is neutropenic, they may be more likely to get infections. When the body cannot fight an infection very well, a child may quickly become seriously ill. Often, a fever is the only sign of infection in a child with neutropenia. For this reason, a fever is considered a medical emergency.
Treating neutropenia
Some patients need medicines to help build up neutrophils that have been destroyed by strong neuroblastoma treatments. These medicines may be given in the hospital, clinic, or home. Your healthcare team will let you know if your child needs one of these medicines.
If your child is neutropenic, your child’s healthcare team may delay certain treatments (chemotherapy) until the neutrophil count rises.
If your child becomes ill or has a fever, they may need to be admitted to the hospital for antibiotics and to be closely monitored by the healthcare team. Do not give your child medication to treat the fever unless you are told to do so by their healthcare team.
Managing neutropenia at home
Keeping your child healthy and safe is key. Not all infections can be prevented when your child has a low neutrophil count, but good hygiene practices can help avoid some. Some precautions you can take to help protect your child from the common causes of infection include:

Please call your healthcare team immediately if your child has a fever or chills, or you are concerned they may have an infection.
Learn about the signs and symptoms of other common side effects of treatment and how the healthcare team may manage each.